Read more
Blog, Rights, protection and inclusion
Improving health through retaining livelihoods: why refugee policy cannot ignore animals
The movement of Ukrainian refugees and their pets across Europe’s borders unleashed an unprecedented solidarity with refugee animals, including the temporary lifting of transboundary veterinary requirements. Common responses to forced migration rarely facilitate or...
In this blog we draw from our research findings published in the journal BMC Public Health to argue that there are strong reasons to expand access to health care services for undocumented immigrants. This is because our study of the mortality of undocumented immigrants in Switzerland as well as across different Swiss cantons shows an important difference in the patterns of mortality of undocumented immigrants compared to other groups of the population. We also find an association between inclusive cantonal health care policies and better health-outcomes for undocumented immigrants. Our research shows the importance of the political determinants of the health of undocumented migrants.
This issue matters because legal precarity and socio-economic marginalization mean that undocumented immigrants are exposed to particularly high health threats. This makes their access to health care services especially important. Yet, availability of care that goes beyond emergency provision – such as screening and preventive treatment for infectious diseases – is available for undocumented migrants only in some cities/countries or specific situations.
The mortality of undocumented immigrants
The data that we used is from the Swiss database of mortality for the period 2011-2017. Within this database, we identify the individuals who are likely to have had undocumented residence status in Switzerland at the time of death; and we compare their patterns of mortality (meaning, the distribution of different causes of death among those who have died) to those of Swiss citizens and regular immigrants.
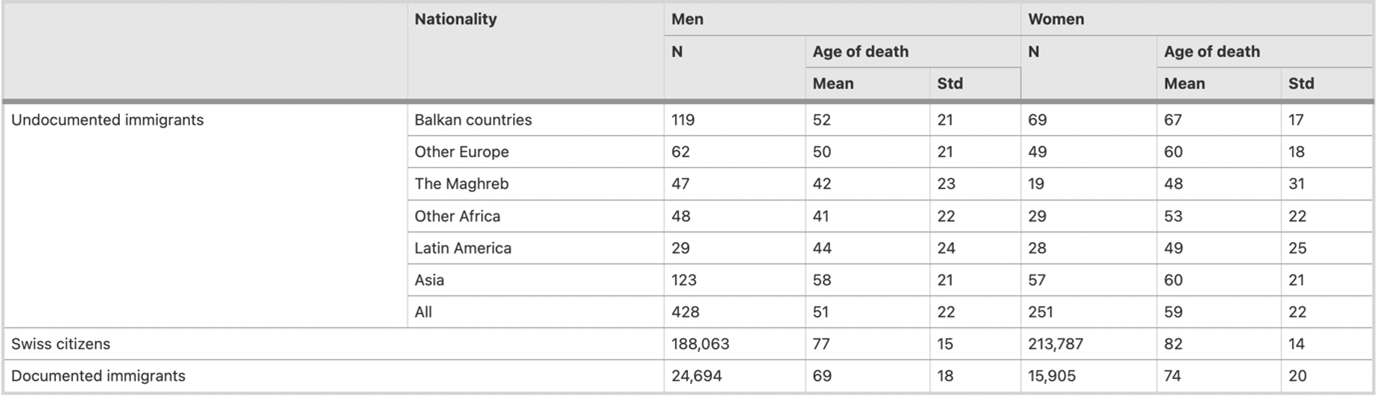
We find some remarkable differences. Table 1 shows that the mean age of death of undocumented immigrants is significantly lower (mean age at death: 54) than it is for documented immigrants (71) and for Swiss citizens (80).
Table 1. Size and age of death of the deceased population per status, nationality and sex
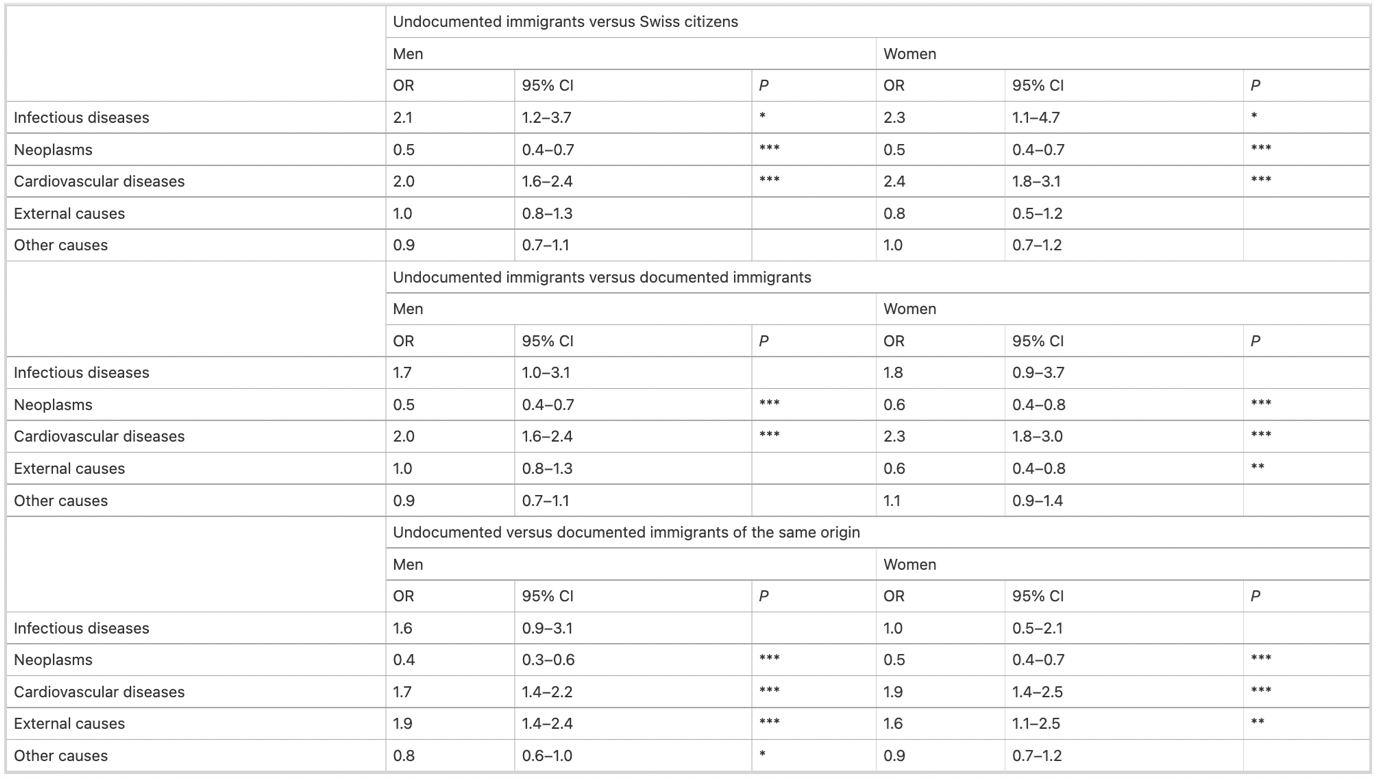
Looking at the causes of mortality through simple regressions, we see that death from circulatory system diseases and cardiovascular diseases is twice as frequent among undocumented immigrants compared to both documented immigrants and Swiss citizens.
Table 2. Odds ratios of mortality for different causes of undocumented immigrants compared to Swiss citizens, documented immigrants, and documented immigrants of the same origin, adjusted for age
We interpret these differences with prudence because they could be partially explained by the different age structure of the various groups of the population. Regrettably, we do not have precise information on the age structure of undocumented immigrants in Switzerland.
The consequences of inclusive health care policies
As a second step, we study whether there is an association between cantonal authorities’ policies and differing mortality patterns. Switzerland has twenty-six cantons that provide various levels of health services for undocumented immigrants. More inclusive health care policies protect undocumented immigrants’ health in many ways. For example, public authorities may formally extend health care coverage to undocumented immigrants and promote more accessible insurance coverage. Lower financial barriers to health insurance and greater access to hospitals and doctors can further facilitate inclusion into the public health care system. Dedicated outreach activities may convince undocumented immigrants to seek health care by moderating problems related to income disparity, fear of deportation, lack of familiarity with the local health care system, shortage of providers who speak their language, and discriminatory treatment by health practitioners. By reducing these barriers, inclusive policies may be conducive to better health status for undocumented immigrants.
Based on existing studies on Swiss cantonal health policies towards undocumented immigrants, we identify three groups of cantons: those with inclusive policies, those with fragmented policies, and those with no policy in place.
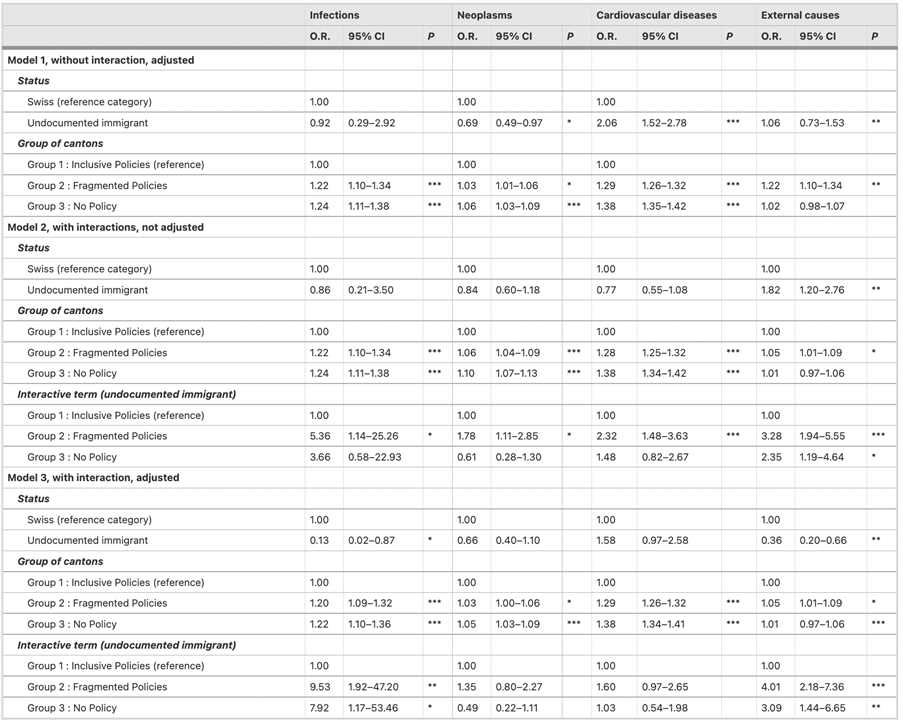
Using simple regressions again, we observe that in cantons with inclusive policies undocumented male mortality from cardiovascular diseases among undocumented immigrants is less than twice as frequent as that of Swiss citizens, whereas in cantons with no policies it is more than twice as frequent. Multinomial analysis confirms that mortality from cardiovascular diseases is more frequent for undocumented immigrants compared to Swiss citizens; but this analysis also shows that the cantonal differences in undocumented immigrants’ mortality from cardiovascular diseases are not statistically significant. By contrast, as Table 2 shows, the odds ratios of undocumented immigrants’ death caused by infectious diseases and death by external causes are significantly higher – and statistically significant – in cantons with fragmented policies and in cantons with no policy than they are in cantons with inclusive policies. Table 3 shows that the difference in mortality patterns between undocumented immigrants and Swiss citizens is generally smaller in the Swiss cantons that have more inclusive health care policies towards undocumented migrants.
Table 3. Multinomial logistic regression with odds ratios of dying from infections, neoplasms, cardiovascular diseases, and external causes compared to other causes of death
Conclusions: the political determinants of the health of undocumented immigrants
Our analysis suggests that policies that expand access to health services lead to better outcomes for undocumented immigrants. We call this the ‘The political determinants of the health of undocumented immigrants’. Evidence of an association between inclusive health care policies towards undocumented immigrants and their health outcomes is especially crucial against the backdrop of the COVID-19 pandemic when there was renewed urgency to create a strong evidence base explaining whether and how inclusive health care policies help to tackle these vulnerabilities.